
Healthcare Shared Decisions is extending our focus on COVID19 with a new series of posts that support you in making your own decisions related to risk.
Using a wildfire to describe the US spread of COVID19 seems apt this summer. Wildfires can begin small and unseen. They are often human driven. When the environment is right they can burst into an inferno in minutes. Even the Big Burn by Timothy Egan, recounting a historical wildfire seems to capture our current response to the pandemic:
“For days, people had watched it [fire on Bitterroot Mountain] from their gabled houses, from front porches and ash-covered streets, and there was some safety in the distance, some fascination even—see there way up on the ridgeline, just like candles flickering in the trees”
Back in 1910, the fire’s environment suddenly changed, and it erupted with a fury that consumed millions of acres, completely destroying many towns, and killing 87 residents and firefighters.
Not Dangerous?
 Like those folks who lost everything by viewing the fire from the perceived safety of their town, many people in America see the virus as a distant event, inconvenient but not dangerous. They say, “I want my life back,” “Only old people die,” and “It’s just like the flu, no big deal.”
Like those folks who lost everything by viewing the fire from the perceived safety of their town, many people in America see the virus as a distant event, inconvenient but not dangerous. They say, “I want my life back,” “Only old people die,” and “It’s just like the flu, no big deal.”
Herein lies the risk to other people. These same folks don’t believe they can infect someone else. Who wants to wear a stupid mask? Social distance, another silly idea because I like being close to the people I talk with – they are fine and so am I. Sure, COVID19 is harmless… like a wildfire!
The amount of scientific content on this virus grows exponentially as clinicians and scientists collaborate around the globe to grasp the long-term effects of COVID19. Without a clear guide and evidence-based information, it’s easy to be swayed by trending stories and click-bait headlines.
No Big Deal: How We Can Fight COVID with the Tools We Have On Hand
Science as Your Compass
 Scientific research results can be a guide for your personal decisions related to risk for yourself and those you love. Each of the following topics will be covered in posts in the coming weeks, with up-to-minute-information. Subscribe to read them all!
Scientific research results can be a guide for your personal decisions related to risk for yourself and those you love. Each of the following topics will be covered in posts in the coming weeks, with up-to-minute-information. Subscribe to read them all!
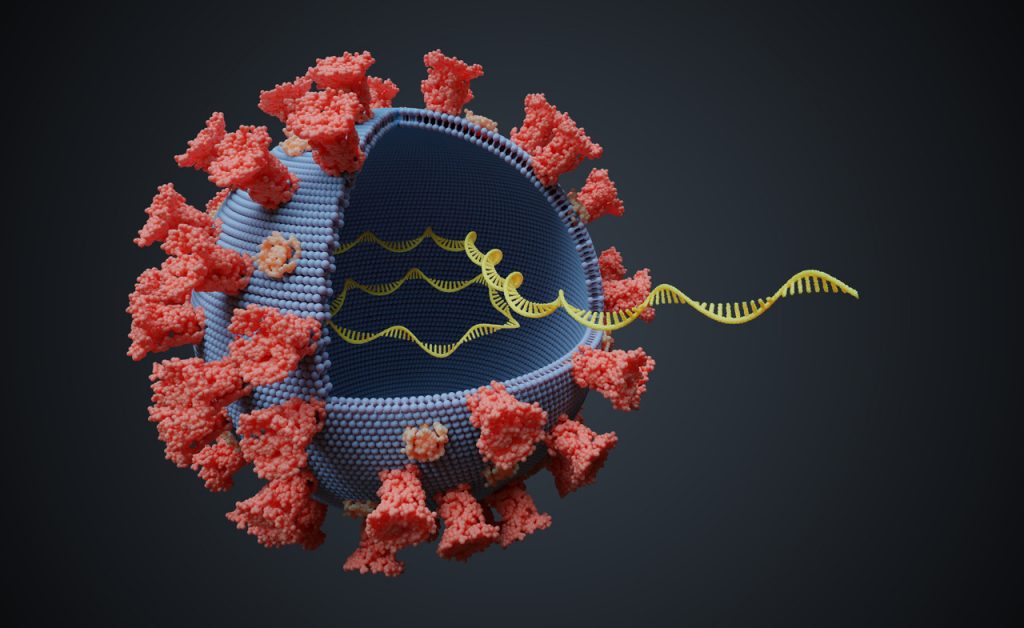
The virus genome is changing.
Implications of this change are in the early stage of evaluation by researchers. Initial work indicates the potential for COVID 19 to become more infectious.
Testing, contact tracing and quarantine have been proven to control COVID19.
Unlike many other countries, the US does not have a coordinated national plan for managing a pandemic, where test, trace and quarantine are the starting point.
New evidence disproves early reports that the elderly and those with co-morbid diagnosis are the only people who are seriously affected by COVID 19.
Today the rising numbers of those with infections are the 18-40 age range. In California the 18-34 age group has 90,322 infections (largest number in the state accounting for 33.2% of the state’s rate, as of July 5th). Children are also affected, with more than 1,000 cases requiring hospitalization and critical care.
Men, people of Hispanic and Black ethnicity, and those with lower socio-economic level experience more severe effects of COVID19.
Why? Data is emerging pointing to answers.
Symptoms are variable and often non-specific.
Recent report from medical journals the link to neurological symptoms may be related to the way the virus enters the lung cells on ACE 2 and this enzyme is also found in neurons.
Long term effects.
The long term effects of this disease are beginning to emerge in the studies related to lung damage, cardiac damage, and neurologic damage.
 Vaccine trials are underway.
Vaccine trials are underway.
Phase II and III trials with several thousands of people enrolled are underway. These will test the potential for side effects as well the ability to protect the person against COVID 19.
Pregnancy and the risk of COVID19 are still unknown right now.
Limited scientific data on how the virus affects the mother, the placenta and the fetus are a few individual case reports, however a multi-center research study is underway.
Immunity after exposure is unknown at this point.
There is another large study underway from the University of Cambridge in collaboration with Australia and New Zealand on antibodies to the virus from those infected.
Subscribe now to be notified of new posts on Shared Decisions

Leave a Reply